Situation Summary
THIS ARTICLE HAS BEEN TAKEN DIRECTLY FROM THE CDC WEBSITE. PLEASE VISIT THEIR SITE HERE FOR MORE UPDATES AND INFORMATION ON CORONAVIRUS
This is a rapidly evolving situation and CDC will provide updated information and guidance as it becomes available.
Updated April 7, 2020
CDC is responding to a pandemic of respiratory disease spreading from person-to-person caused by a novel (new) coronavirus. The disease has been named “coronavirus disease 2019” (abbreviated “COVID-19”). This situation poses a serious public health risk. The federal government is working closely with state, local, tribal, and territorial partners, as well as public health partners, to respond to this situation. COVID-19 can cause mild to severe illness; most severe illness occurs in adults 65 years and older.
Situation in U.S.
Different parts of the country are seeing different levels of COVID-19 activity. The United States nationally is in the acceleration phase of the pandemic. The duration and severity of each pandemic phase can vary depending on the characteristics of the virus and the public health response.
- CDC and state and local public health laboratories are testing for the virus that causes COVID-19. View CDC’s Public Health Laboratory Testing map.
- All 50 states have reported cases of COVID-19 to CDC.
- U.S. COVID-19 cases include:
- Imported cases in travelers
- Cases among close contacts of a known case
- Community-acquired cases where the source of the infection is unknown.
- All U.S. states are reporting some community spread of COVID-19.
- View latest case counts, deaths, and a map of states with reported cases.
On This Page
- Situation in U.S.
- CDC Recommends
- COVID-19 Background
- Severity
- COVID-19 Now a Pandemic
- Risk Assessment
- CDC Response
- Highlights of CDC’s Response
- Other Available Resources
Confirmed COVID-19 Cases Global Map
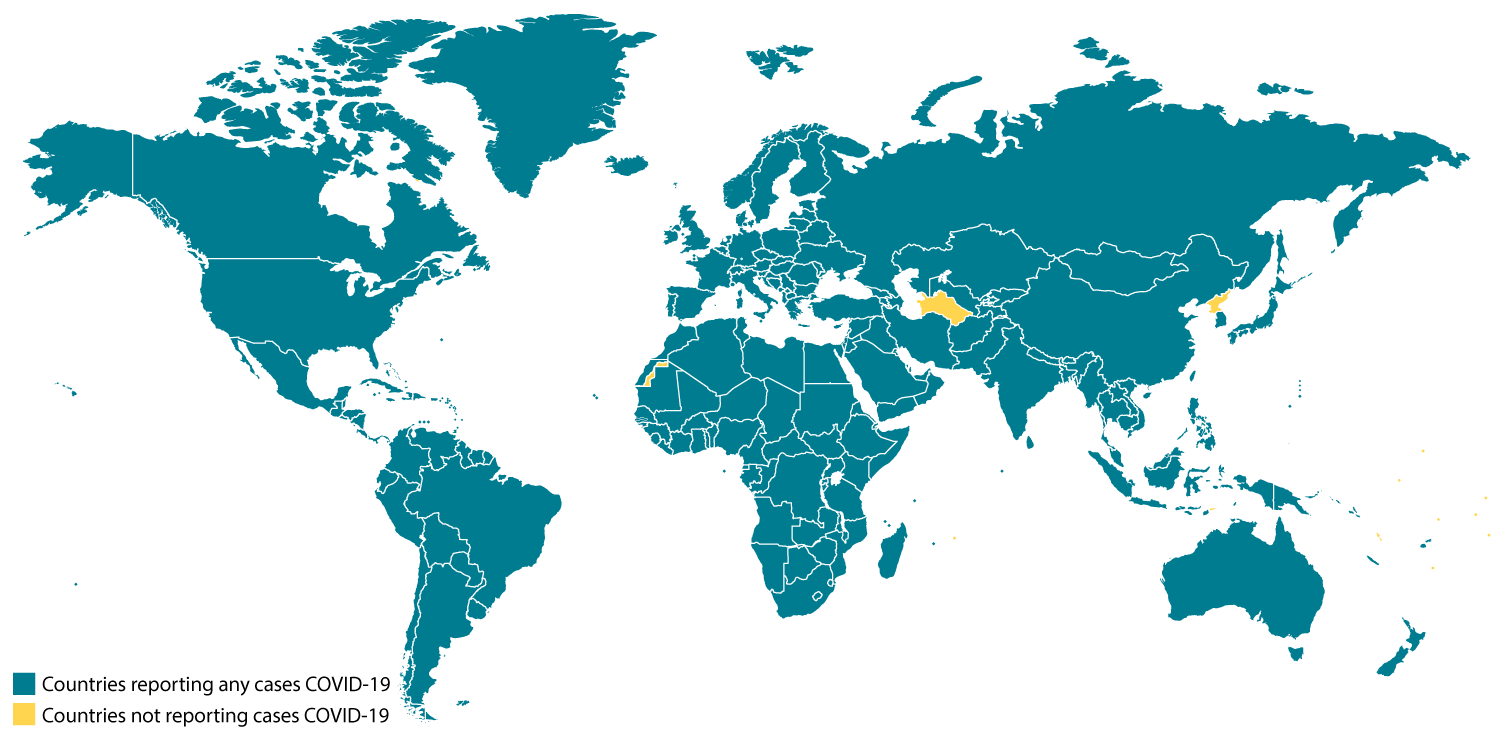
View larger image and see a list of locationsmap icon
COVID-19 cases in the U.S.
CDC Recommends
- Everyone can do their part to help us respond to this emerging public health threat:
- CDC is recommending the use of a cloth face covering to keep people who are infected but do not have symptoms from spreading COVID-19 to others.
- The cloth face cover is meant to protect other people in case you are infected.
- The cloth face coverings recommended are not surgical masks or N-95 respirators. Medical face masks are critical supplies that should be reserved for healthcare workers and other first responders, as recommended by CDC.
- The cloth face cover is not a substitute for social distancing.
- CDC continues to recommend that people try keep about 6 feet between themselves and others.
- The White House “Slow the Spread” guidelinespdf iconexternal icon are in place until April 30. These are part of a nationwide effort to slow the spread of COVID-19 through the implementation of social distancing at all levels of society.
- People 65 years and older and people with severe underlying medical conditions should take special precautions because they are at higher risk of developing serious COVID-19 illness.
- If you are a healthcare provider, use your judgment to determine if a patient has signs and symptoms compatible with COVID-19 and whether the patient should be tested. CDC’s Criteria to Guide Evaluation and Laboratory Testing for COVID-19 provides priorities for testing patients with suspected COVID-19 infection.
- People who get a fever or cough should consider whether they might have COVID-19, depending on where they live, their travel history or other exposures. All of the U.S. is seeing some level of community spread of COVID-19. Testing for COVID-19 may be accessed through medical providers or public health departments, but there is no treatment for this virus. Most people have mild illness and are able to recover at home without medical care.
- American citizens, lawful permanent residents, and their families who have been in one of the countries with travel restrictions for entering the U.S. in the past 14 days will be allowed to enter the United States but will be redirected to one of 13 airports. If you are returning from one of these countries, you should stay home and monitor your health. All other international travelers please follow CDC instructions during this time. Your cooperation is integral to the ongoing public health response to try to slow spread of this virus.
COVID-19 Background
COVID-19 is caused by a new coronavirus. Coronaviruses are a large family of viruses that are common in people and many different species of animals, including camels, cattle, cats, and bats. Rarely, animal coronaviruses can infect people and then spread between people such as with MERS-CoV, SARS-CoV, and now with this new virus (named SARS-CoV-2).
The SARS-CoV-2 virus is a betacoronavirus, like MERS-CoV and SARS-CoV. All three of these viruses have their origins in bats. The sequences from U.S. patients are similar to the one that China initially posted, suggesting a likely single, recent emergence of this virus from an animal reservoir.
Early on, many of the patients at the epicenter of the outbreak in Wuhan, Hubei Province, China had some link to a large seafood and live animal market, suggesting animal-to-person spread. Later, a growing number of patients reportedly did not have exposure to animal markets, indicating person-to-person spread. Person-to-person spread was subsequently reported outside Hubei and in countries outside China, including in the United States. Most international destinations now have ongoing community spread with the virus that causes COVID-19, as does the United States. Community spread means some people have been infected and it is not known how or where they became exposed. Learn more about the spread of this coronavirus that is causing COVID-19.
Severity
The complete clinical picture with regard to COVID-19 is not fully known. Reported illnesses have ranged from very mild (including some with no reported symptoms) to severe, including illness resulting in death. While information so far suggests that majority of COVID-19 illnesses are mild. An early reportexternal icon out of China found serious illness in 16% of cases. A CDC Morbidity & Mortality Weekly Report that looked at severity of disease among COVID-19 patients in the United States by age group found that 80% of deaths were among adults 65 years and older with the highest percentage of severe outcomes occurring in people 85 years and older. People with serious underlying medical conditions — like serious heart conditions, chronic lung disease, and diabetes, for example — also seem to be at higher risk of developing serious COVID-19 illness.
Learn more about the symptoms associated with COVID-19.
COVID-19 Pandemic
A pandemic is a global outbreak of disease. Pandemics happen when a new virus emerges to infect people and can spread between people sustainably. Because there is little to no pre-existing immunity against the new virus, it spreads worldwide.
The virus that causes COVID-19 is infecting people and spreading easily from person-to-person. On March 11, the COVID-19 outbreak was characterized as a pandemic by the WHOexternal icon.
This is the first pandemic known to be caused by a new coronavirus. In the past century, there have been four pandemics caused by the emergence of new influenza viruses. As a result, most research and guidance around pandemics is specific to influenza, but the same premises can be applied to the current COVID-19 pandemic. Pandemics of respiratory disease follow a certain progression outlined in a “Pandemic Intervals Framework.” Pandemics begin with an investigation phase, followed by recognition, initiation, and acceleration phases. The peak of illnesses occurs at the end of the acceleration phase, which is followed by a deceleration phase, during which there is a decrease in illnesses. Different countries can be in different phases of the pandemic at any point in time and different parts of the same country can also be in different phases of a pandemic.

Source: CDC’s “Updated Preparedness and Response Framework for Influenza Pandemics.”.
Risk Assessment
Risk depends on characteristics of the virus, including how well it spreads between people; the severity of resulting illness; and the medical or other measures available to control the impact of the virus (for example, vaccines or medications that can treat the illness) and the relative success of these. In the absence of vaccine or treatment medications, nonpharmaceutical interventions become the most important response strategy. These are community interventions that can reduce the impact of disease.
The risk from COVID-19 to Americans can be broken down into risk of exposure versus risk of serious illness and death.
Risk of exposure:
- Cases of COVID-19 and instances of community spread are being reported in all states.
- People in places where ongoing community spread of the virus that causes COVID-19 has been reported are at elevated risk of exposure, with the level of risk dependent on the location.
- Healthcare workers caring for patients with COVID-19 are at elevated risk of exposure.
- Close contacts of persons with COVID-19 also are at elevated risk of exposure.
- Travelers returning from affected international locations where community spread is occurring also are at elevated risk of exposure, with level of risk dependent on where they traveled.
Risk of Severe Illness:
Based on currently available information and clinical expertise, older adults and people of any age who have serious underlying medical conditions might be at higher risk for severe illness from COVID-19. Based on what we know now, those at higher risk for severe illness from COVID-19 are:
- People 65 years and older
- People who live in a nursing home or long-term care facility
- People of all ages with underlying medical conditions
CDC has developed guidance to help in the risk assessment and management of people with potential community-related exposures to COVID-19.
CDC Response
Global efforts at this time are focused concurrently on lessening the spread and impact of this virus. The federal government is working closely with state, local, tribal, and territorial partners, as well as public health partners, to respond to this public health threat.
Highlights of CDC’s Response
- CDC established a COVID-19 Incident Management System on January 7, 2020. On January 21, CDC activated its Emergency Operations Center to better provide ongoing support to the COVID-19 response.
- The U.S. government has taken unprecedented steps with respect to travel in response to the growing public health threat posed by this new coronavirus:
- Foreign nationals who have been in China, Iran, the United Kingdom, Ireland and any one of the 29 European countries in the Schengen Area within the past 14 days cannot enter the United States.
- U.S. citizens, residents, and their immediate family members who have been any one of those countries within in the past 14 days can enter the United States, but they are subject to health monitoring and possible quarantine for up to 14 days.
- CDC has issued a Level 3 Travel Health Notice for cruise ship travel. CDC recommends that all people defer travel on cruise ships, including river cruises, worldwide.
- CDC has issued additional specific travel guidance related to COVID-19.
- CDC has issued clinical guidance, including:
- Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19).
- Infection Prevention and Control Recommendations for Patients, including guidance on the use of personal protective equipment (PPE) during a shortage.
- CDC also has issued guidance for other settings, including schools, workplaces and community locations.
- A collection of CDC’s COVID-19 Guidance Documents can be found online.
- CDC has deployed multidisciplinary teams to support state health departments in case identification, contact tracing, clinical management, and public communications.
- CDC has worked with federal partners to support the safe return of Americans overseas who have been affected by COVID-19.

This is a picture of CDC’s laboratory test kit for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). CDC tests are provided to U.S. state and local public health laboratories, Department of Defense (DoD) laboratories.resize iconView Larger
- An important part of CDC’s role during a public health emergency is to develop a test for the pathogen and equip state and local public health labs with testing capacity.
- CDC developed an rRT-PCR test to diagnose COVID-19.
- As of the evening of April 13, 95 state and local public health labs in 50 states, the District of Columbia, Guam, and Puerto Rico have successfully verified and are currently using CDC COVID-19 diagnostic tests.
- Commercial manufacturers are now producing their own tests.
- CDC has grown the COVID-19 virus in cell culture, which is necessary for further studies, including for additional genetic characterization. The cell-grown virus was sent to NIH’s BEI Resources Repositoryexternal icon for use by the broad scientific community.
- CDC also is developing a serology test for COVID-19.
Other Available Resources
The following resources are available with information on COVID-19